Polysensitization in Contact Allergy in Benin: Study of Three Cases
Akpadjan F, Adégbidi H, Koudoukpo C, Dégboé B, Kouotou EA, Agbessi N and Atadokpèdé F
Akpadjan F1*, Adégbidi H1, Atadokpèdé F1, Dégboé B1, Koudoukpo C2, Agbessi N2 and Kouotou EA3
1Department of Health Sciences, Cotonou, UAC, Benin
2Department of Medicine of Parakou, UP, Benin
3Department of Medicine and Biomedical Sciences, University of Yaounde, Cameroon
- Corresponding Author:
- Akpadjan F
Department of Health Sciences
Cotonou, UAC, Benin
Tel: 97074409
E-mail: barfice@yahoo.fr
Received Date: September 19, 2016; Accepted Date: September 25, 2016; Published Date: September 29, 2016
Citation: Akpadjan F, Adégbidi H, Atadokpèdé F, Dégboé B, Koudoukpo C, et al. (2016) Polysensitization in Contact Allergy in Benin: Study of Three Cases. J Allergy Inflamm 2: 1.
Copyright: © 2017 Akpadjan F, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Periodically updated (from 23 to 28 allergens), the European baseline series (EBS), first introduced in France in 1980, is an indispensable tool for the exploration of contact allergy. Patients with multiple contact allergies, also referred to as polysensitized, are more frequent than predicted from prevalence of single sensitivities.
Observations: There were three cases of patch tests carried out respectively in a 3 ½ years, a 37 year old woman and a man of 53 years. All three patients had polysensitization six contact allergens.
Discussion: This is a first study conducted in Benin on allergenic polysensitization. These three cases show that polysensitization can be seen in the child as well as the adult on the one hand, and in both sexes on the other.
Keywords
Contact allergy; Patch tests; Polysensitization; Benin
Introduction
Periodically updated (from 23 to 28 allergens), the European baseline series (EBS), first introduced in France in 1980, is an indispensable tool for the exploration of contact allergy [1].
Patients with allergic contact dermatitis to 1 antigen are at an increased risk of developing delayed type hypersensitivity reactions to additional antigens. Both environmental and genetic factors likely influence the risk of sensitization [2].
Contact allergy to several non-related haptens, usually termed polysensitization (PS), is often used to characterize patients who are particularly prone to sensitization. Polysensitization may be regarded as a special entity in patients with contact allergies. However, this group of polysensitized patients is poorly characterized.
Filaggrin mutations are associated with atopic eczema and lead to impaired skin barrier which may predispose to contact allergy.
Therefore, it is of interest to consider atopic eczema and contact allergies, especially in patients with multiple allergies [3]. The literature supports the idea that patients with multiple contact allergies constitute a special entity within the field of contact allergy.
There is no generally accepted definition of patients with multiple contact allergies. A conventional definition for PS is positive reactions to three or more haptens of the baseline series [4,5]. To date, no studies have been carried out in Benin on polysensitization in contact allergy.
We report here the first study on this subject in our country. All patients had been tested in a dermatology clinic by the European Standard Series composed of 28 allergens.
Observations
Case 1
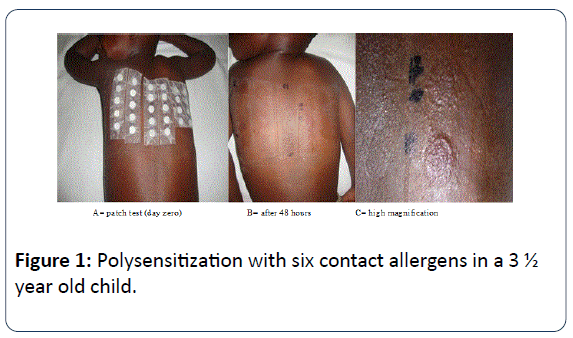
A 3 ½ years old child was followed as early as 03 months of age for recurrent eczema sometimes erythrodermic. The interrogation found a personal and family atopy. Crises were well controlled by weak dermocorticoids. But in the face of this recurrent chronic course, a patch test was carried out with the European Standard Series (ESS).
The reading was done at 48th hour and 96th hour. At the end of 96 hours of reading, it was observed a positivity for six allergens: N-isopropyl-N'-phenylparaphenylene diamine 0.1%, Fragrance mix 8%, Fragrance mix 14%, colophony, Paraphenylene diamine 1% and Cl+ME-isothiazolinone 0.01%.
Relevance of these allergens investigation was carried out and was positive. The child's mother was using everyday products containing several different allergens identified. Removing these allergens for this child has achieved a permanent cure his eczema (Figure 1).
Case 2
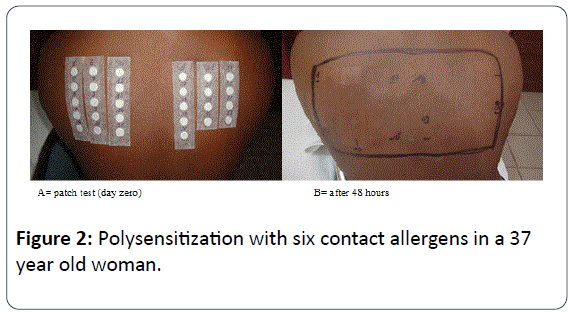
A Catholic nun 37 years old woman was referred by his dermatologist for producing a patch test. The patient was followed by the latter for chronic atopic dermatitis recurring for several years. Crises were not well controlled by different therapeutics available in Benin. The interrogation found a personal atopy made of asthma and allergic rhino sinusitis. The patch-test carried out with the European Standard Series allowed to observe a positivity for six allergens: Potassium dichromate 0.5%, Balsam of Peru 25%, N-Isopropyl-N'- phenylparaphenylenediamine 0.1%, Paraben-mix 12%, Sesquiterpene lactone mix 0.1% and Tixocortol pivalate 1% (Figure 2).
Relevance of these allergens investigation was carried out and was also positive. The patient wore leather or rubber shoes on the one hand and she regularly used throat lozenges, cough suppressants and nasal sprays to relieve her sinusitis. There are also cross-reactions between Tixocortol and Balsam of Peru. The removal of most of these allergens by the patient has greatly reduced her eczema attacks. Complete remission is not yet achieved because of these allergens contained in the products used for the treatment of rhino sinusitis; as substitute products have not yet been found.
Case 3
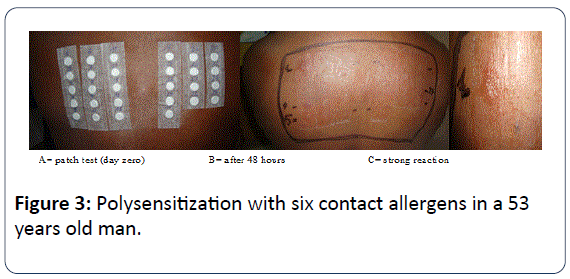
A 53 years old man with a personal history of atopy was sent by his dermatologist treating for carrying out a patch test. The patient suffered from chronic recurrent eczema of the feet and hands. The patch-test carried out with the European Standard Series allowed to objectify also a positivity for six allergens: Potassium dichromate 0.5%, Paraphenylene diamine 1%, Cobalt chloride 1%, Dibromodicyano-butane 0.3%, Balsam of Peru 25%, Budesonide 0.1% (Figure 3).
Relevance of these allergens has also been proven. With the patient forestry profession is subject to daily wear closed shoes leather which explains the strong reaction to Potassium dichromate 0.5%.
Also note a cross-reaction between Potassium dichromate and paraphenylene diamine. The removal of most of these allergens has greatly reduced eczema attacks.
The difficulty encountered in the therapeutic management of this patient is related to the choice of topical corticosteroids to use because most of them present cross-reactions with Budesonide (Table 1).
| Positive allergens | Results | |||
|---|---|---|---|---|
| N° | Names | 48h | 96h | |
| Case 1 | 4 | Paraphenylenediamine (1%) | + | ++ |
| 8 | Colophony (20%) | + | ++ | |
| 11 | N-Isopropyl-N’Phenylparaphenylenediamine (0.1%) | + | + | |
| 17 | Fragrance Mix (8%) -Sorbitansesquioleate (5%) | ++ | ++ | |
| 18 | Fragrance Mix (14%) | +++ | ++ | |
| 22 | Cl+ME- isothiazolinone (0.01%) | + | ++ | |
| 1 | Potassium dichromate (0.5%) | ++ | + | |
| 10 | Balsam of Peru (25%) | ++ | + | |
| 11 | N-Isopropyl-N’Phenyl-paraphenylenediamine (0.1%) | ++ | + | |
| Case 2 | 15 | Paraben-Mix (12%) | ++ | + |
| 19 | Sesquiterpene lactone Mix (0.1%) | ++ | + | |
| 28 | TixocortolPivalate (1%) | ++ | + | |
| 1 | Potassium dichromate (0.5%) | +++ | +++ | |
| 4 | Paraphenylenediamine (1%) | ++ | + | |
| 5 | Cobalt chloride (1%) | ++ | + | |
| Case 3 | 10 | Balsam of Peru (25%) | ++ | + |
| 26 | Budesonide (0.1%) | + | ++ | |
| 27 | Dibromodicyanobutane (0.3%) | ++ | + | |
Table 1: Different allergens positive in our three patients.
Discussion
This is a first study in Benin on polysensitization contact allergy. These three cases show that polysensitization can be seen in both the child and the adult on the one hand and in both sexes on the other. This confirms the literature data [6]. Very few studies have focused on the sensitization of children to contact allergens. This case of polysensitization in our child (Case 1), however, shows cross-reactions one hand between N-Isopropyl- N'-phenyl-paraphenylene diamine 0.1% and Paraphenylenediamine 1%, on the other hand between the fragrance mix 8% and 14%. Note that the higher the percentage of fragrance, the sharper the reaction. Also the different allergens are found in the immediate environment of our child every day; these are essentially rubber, leather, adhesives and scented products. The eviction of these identified allergens applies both to the child but also the parents especially the mother using scented products. In the case of cash the family has simply moved to another city of Benin. This has made it possible to note that for nearly two years of follow-up, the child has no longer had an eczema crisis. Note that all three patients share at least one positive allergen.
Retrospective studies demonstrate that the prevalence of skin sensitization does not significantly differ between atopic and non-atopic patients. In children and adolescents the risk for sensitization seems to occur independently from atopic dermatitis (AD). According to the results of a recent study, AD patients are overrepresented in the group of polysensitized patients [7]. In this study we observed that all three patients had atopic terrain.
Patients with multiple contact allergies have received limited research focus. Knowledge about patients with multiple contact allergies mainly relies on a few studies and general perceptions. Patients with multiple contact allergies probably do exhibit a special entity in the field of contact allergies as the observed frequency exceeds the predicted frequency in both general and eczema populations [8]. In a recent study of risk factors for polysensitization, it was found that regarding an anatomical sites as exposure (surrogate), the axillae and the feet were found to be strong PS risk factors. Moreover, age was a strong PS risk factor, and less so, female sex. In comparison, atopic eczema and occupational dermatitis were less important risk factors. Single allergens contributed to PS to a varying extent [9]. Our three clinical cases simply show that PS can affect both sexes and all ages.
The purpose of this study is to draw attention to the existence of these cases of polysensitization although rare, under our skies. It is therefore necessary to think especially in the case of recurrent chronic eczema, despite a well-conducted treatment. It will also be necessary to systematically request the realization of patch test in these patients at risk of polysensitization.
The limitations of our study concern mainly the reduced number of polysensitized patients in Benin. This does not allow us to conduct an in-depth epidemiological study at this time. Berit Christina Carlsen's 2009 thesis entitled "Patients with multiple contact allergies: Population characteristics and clinical presentation" draws the following conclusions regarding the epidemiological and clinical characteristics of polysensitized patients: The frequency of polysensitization over 20 years was stable. The prevalence was 5.1%. Four out of 5 with multiple contact allergies were women and the risk of polysensitization increased with increasing age; 90% were diagnosed with multiple contact allergies at the first patch test in the hospital sector. When repeating the patch test, the risk of multiple contact allergies increased. Those allergens that are known to be frequent causes of contact allergy were also frequent causes among patients with multiple contact allergies and vice versa for the rare allergens. In patients with multiple contact allergies, 45% had had atopic eczema, whereas the occurrence of leg ulcers was low. The hands were the body part which was affected with dermatitis most frequently at time of debut. Patients with multiple contact allergies did not have more widespread dermatitis than did patients with 1-2 contact allergies. Atopic eczema and hand dermatitis were positively associated with polysensitization. Neither specific educational levels nor leg ulcers increased the risk of polysensitization. Other body parts were also, respectively, positively and negatively associated with polysensitization, but this was not as consistent as with hand dermatitis. The number of contact allergies had a different influence on duration and course of disease among patients with and without atopic eczema, respectively [10].
Conclusion
Contact allergy is a delayed-type hypersensitivity reaction triggered by direct skin contact with low-molecular weight molecules in the environment. Contact allergy is generally perceived as being life- long, and patients are advised to avoid specific allergens for the rest of their lives. These three clinical cases allow us to notice that the polysensitization can be observed at any age and in both sexes. The contact allergy deserves an exploration by the systematic patch tests especially before chronic and recurrent of atopic dermatitis; The association of the two aetiological factors (atopic dermatitis and contact eczema) is indeed a reality. In this study we observed that all three patients had atopic terrain. It is made clear that patients with a genetic predisposition to allergy have a greater risk to polysensitization. These case polysensitization are uncommon in the world in general and Benin in particular where the four years of implementation of patch tests on fifty patients, only three cases have been found.
Eviction measures adapted to the allergological assessment always improve the condition of patients with contact dermatitis and atopic eczema.
References
- Schoeffler A, Waton J, Latarche C, Poreaux C, Cuny JF, et al. (2013) Evolution of the european standard battery from 1981 to 2011 in a French dermato-allergologycenter. Ann DermatolVenereol 140: 499-509.
- Gosnell AL, Schmotzer B, Nedorost ST (2015) Polysensitization and individual susceptibility to allergic contact dermatitis. Dermatitis 26: 133-135.
- Carlsen BC, Andersen KE, Menné T, Johansen JD (2009) Characterization of the polysensitized patient: A matched case-control study. Contact Dermatitis61: 22-30.
- Schwitulla J, Uter W (2015) Multiple Contact sensitization. Der Hautarzt66: 680-685.
- Carlsen BC, Andersen KE, Menné T, Johansen JD (2008) Patients with multiple contact allergies: A review. Contact Dermatitis58: 1-8.
- De Waard-Van Der Spek FB, Oranje AP (2009) Patch tests in children with suspected allergic contact dermatitis: A prospective study and review of the literature. Dermatology218: 119-125.
- Niebuhr M, Kapp A, Werfel T, Heratizadeh A (2011) Allergic contact dermatitis and atopy. Der Hautarzt62: 744-750.
- Carlsen BC, Menné T, Johansen JD (2007) 20 Years of standard patch testing in an eczema population with focus on patients with multiple contact allergies. Contact Dermatitis57: 76-83.
- Schwitulla J, Gefeller O, Schnuch A, Uter W (2013) Risk factors of polysensitization to contact allergens. Br J Dermatol169:611-617.
- Carlsen BC (2009) Patients with multiple contact allergies: Population characteristics and clinical presentation. PhD thesis, Faculty of health sciences university of Copenhagen.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences