A Case of Subcorneal Pustular Dermatosis Successfully Treated with Acitretin
Havva Ozge Keseroglu, Necip Enis Kaya, Aysun Gokce, Muzeyyen Gonul
Havva Ozge Keseroglu1, Necip Enis Kaya1, Aysun Gökçe2 and Müzeyyen Gönül1
1Department of Dermatology, DÃÆââ¬Å¾ÃâñÃÆââ¬Â¦Ãâà ¸kapÃÆââ¬Å¾Ãâñ YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm BeyazÃÆââ¬Å¾Ãâñt Education and Research Hospital, Ankara, Turkey
2Department of Pathology, DÃÆââ¬Å¾ÃâñÃÆââ¬Â¦Ãâà ¸kapÃÆââ¬Å¾Ãâñ YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm BeyazÃÆââ¬Å¾Ãâñt Education and Research Hospital, Ankara, Turkey
- *Corresponding Author:
- Necip Enis Kaya
Department of Dermatology, DÃÆââ¬Å¾ÃâñÃÆââ¬Â¦Ãâà ¸kapÃÆââ¬Å¾Ãâñ YÃÆââ¬Å¾ÃâñldÃÆââ¬Å¾ÃâñrÃÆââ¬Å¾Ãâñm BeyazÃÆââ¬Å¾Ãâñt Education and Research Hospital
06110, Ankara, Turkey
Tel: 90 312 596 2000
E-mail: dr.eniskaya@gmail.com
Received date: August 19, 2016; Accepted date: October 17, 2016; Published date: October 27, 2016
Citation: Keseroglu HO, Kaya NE, Gökçe A, Gönül M (2016) A Case of Subcorneal Pustular Dermatosis Successfully Treated with Acitretin. Arch Inflamm 1:2.
Copyright: © 2016 Keseroglu HO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Subcorneal pustular dermatosis is a rare, chronic neutrophilic dermatoses characterized by recurrent, sterile pustules localized to the trunk, intertriginous regions and flexural surfaces of extremities. The diagnosis of disease is made by demonstration of subcorneal pustules containing neutrophils histopathologically and negative immunofluorescence staining. We reported a 68-year-old male patient with subcorneal pustular dermatosis, who was misdiagnosed as dermatitis herpetiformis without performing direct immunofluorescence examination and had been treated with dapsone with partial benefit for 20 years. He was admitted to our clinic because of the increasing complaints after the cessation of dapsone treatment 2 months before due to development of anemia. The diagnosis of subcorneal pustular dermatosis was made clinically and histopathologically. Complete remission was achieved with systemic acitretin treatment. With this case, we want to emphasize that direct immunofluorescence examination is necessary in order to distinguish subcorneal pustular dermatosis from dermatitis herpetiformis and IgA pemphigus. Acitretin can be a safe and effective treatment option for these patients.
Keywords
Subcorneal pustular dermatosis; Dermatitis herpetiformis; Direct immunofluorescence
Introduction
Subcorneal pustular dermatosis (SPD), Sneddon-Wilkinson disease, is rare chronic neutrophilic dermatoses with unknown etiopathogenesis. It is characterized by flaccid pustules arranged in annular, circinate or serpiginous pattern that is frequently localized to trunk, flexural and intertriginous sites of body with unknown etiopathogenesis. The diagnosis of the disease is made by demonstration of subcorneal pustules containing neutrophils histopathologically and negative immunofluorescence staining [1].
Case
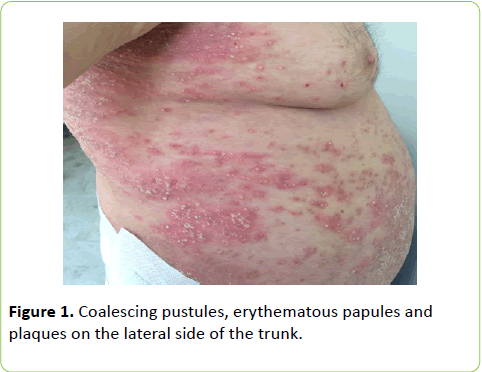
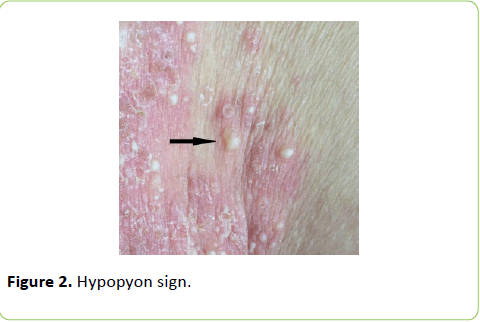
A 68-year-old man was admitted to our clinic with the complaint of blisters containing pus over the body. The lesions had begun on the trunk and legs 20 years before. In that period, the histopathological examination was found to be consisted with dermatitis herpetiformis but direct immunofluorescence (DIF) examination was not performed. The patient had used dapsone treatment with partial benefit for the last 20 years. Five years ago, gluten-free diet was started with the suspicion of Celiac disease. He was admitted to our clinic because of the increasing complaints after the cessation of dapsone treatment 2 months before due to development of anemia. The past investigation records of patient were re-evaluated and it was observed that results of celiac antibodies and colonoscopy were within normal limits. Dermatological examination revealed that coalescing pustules, erythematous papules and plaques which were arranged in annular pattern on erythematous base on the trunk, arms and legs, especially around umbilicus and back. Hypopyon sign was positive for some pustules (Figures 1 and 2).
Laboratory examinations were within normal limits, except for elevation in fasting blood glucose (139 mg/dl, N: 74-106), erythrocyte sedimentation rate (41 mm/h; N: 0-20), C-reactive proteins (61.3 mg/dl, N: 0-8) in addition to anemia (Hb: 10.0 g/dl, N: 13.2-17.3). Histopathological examination of the pustular lesion revealed that subcorneal neutrophilic infiltration, loss of granular layer, acanthosis, spongiosis, dermal edema, lots of polymophonuclear leucocytes around the blood vessels and in interstitial space (Figure 3 and 4).
DIF examination of perilesional skin was negative. The diagnosis of SPD was made clinically and histopathologically. Investigations for concomitant diseases, such as monoclonal gammopathy, inflammatory bowel disease, rheumatoid arthritis, were negative. Systemic acitretin (35 mg/d) treatment was started in addition to single dose triamcinolone acetonide 40 mg injection. Lesions almost completely recovered within two weeks and he has been in remission for 18 months without gluten-free diet.
Discussion
SPD is clinically characterized by recurrent, sterile pustules localized symmetrically on trunk, intertriginous regions and flexor surfaces of the extremities. Pustules, which arise on normal-appearing or erythematous skin, are usually flaccid and show tendency to rupture easily and coalescence. Hypopyon sign is positive usually. Areas of desquamation, crusting and hyperpigmentation may occur with the rupture of pustules [1].
Although the etiopathogenesis of disease is not clear, many theories, including infectious and autoimmune mechanisms, have been proposed [2]. Immune dysfunction due to abnormal cytokine increase was blamed in pathogenesis. Increased amount of TNF-alpha, IL-8, leukotriene B4 in the serum and complement C5 and its metabolites in the extract isolated from pustules were detected [1,3]. IgA monoclonal gammopathy, multiple myeloma and other myeloproliferative disorders are diseases which may accompany with SPD. Concomitant occurrence of subcorneal dermatosis with pyoderma gangrenosum, SAPHO (synovitis, acne, pustulosis, hyperostosis, osteitis) syndrome, Crohn's disease, autoimmune diseases (Sjögren's syndrome, systemic lupus erythematosus), rheumatoid arthritis, hyperthyroidism, apudoma, thymoma, squamous cell carcinoma of lung has rarely been reported, in the literature [1-6]. No concomitant disease was detected in our patient.
Histopathologically, it is characterized by subcorneal pustules containing neutrophils and rarely eosinophils with minimal epidermal changes. Perivascular dermal infiltration can be seen. Direct and indirect immunofluorescence examinations are usually negative [1].
The differential diagnosis of SPD includes pustular psoriasis, impetigo, dermatophyte infections, dermatitis herpetiformis, pemphigus foliaceus, IgA pemphigus and necrolytic migratory erythema. Many of these diseases can be distinguished with the help of native preparation, direct smear and histopathological examination. However, in order to distinguish SPD from IgA pemphigus and dermatitis herpetiformis, DIF examination is necessary in addition to the histopathological examination [1-3]. We couldn’t be sure the past diagnosis of dermatitis herpetiformis due the absence of DIF before.
Dapsone is the first choice in the treatment of SPD. Although most of the patients gives a dramatic response to this treatment, adequate response may not be achieved in some cases. Systemic and topical steroids may be given alone or in combination with dapsone. Sulphapyridine, colchicine, minocycline, cyclosporine and phototherapy are other treatment options [2-6]. There are a few patients treated with acitretin in the literature [5]. In our patient, only partial remission could be achieved with dapsone and this treatment had to be stopped because of anemia. Complete remission was obtained with acitretin treatment.
In conclusion, the diagnosis of SPD should be suspected when neutrophilic microabscesses were seen in histopathology and DIF examination should be done in order to make an accurate diagnosis. Acitretin can be a safe and effective treatment option for the patients who do not respond to dapsone or cannot use it.
References
- Razera F, Olm GS, Bonamigo RR (2011) Neutrophilic dermatoses: part II. An Bras Dermatol 86: 195-209.
- Khachemoune A, Blyumin ML (2003) Sneddon Wilkinson disease resistant to dapsone and colchicine successfully controlled with PUVA. Dermatol Online J 9: 24.
- Ratnarathorn M, Newman J (2008) Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) occurring in association with nodal marginal zone lymphoma: a case report. Dermatol Online J 14: 6.
- Rasch A, Schimmer M, Sander CA (2009) Subcorneal pustulosis with combined lack of IgG/IgM and monoclonal gammopathy type IgA/Kappa. J Dtsch Dermatol Ges 7: 693-696.
- Canpolat F, Akpinar H, Cemil BC, EskioÃÆââ¬Å¾Ãâà ¸lu F, Oztürk E (2010) A case of subcorneal pustular dermatosis in association with monoclonal IgA gammopathy successfully treated with acitretin. J Dermatolog Treat 21: 114-116.
- Prat L, Bouaziz JD, Wallach D, Vignon-Pennamen MD, Bagot M (2014) Neutrophilic dermatoses as systemic diseases. Clin Dermatol 32: 376-388.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences